Local cryotherapy acute soft tissue injury care management, let’s call the POLICE
“Somebody get ICE!” an often used reflex when somebody just sprained his ankle or felt on his wrist. The use of ice or cryotherapy in acute soft tissue injury is a well-known strategy to cope with the first problems of swelling and pain, despite a paucity of scientific data that support this strategy. Throughout the years it became evident that cryotherapy should not be an act on its own but needs to be part of an integral approach.
First, let us tackle a general misconception:
Do you need to limit or eliminate inflammation?
The answer is no, inflammation is necessary. The repair will not occur without inflammation, and even if you want to, you cannot eliminate inflammation; you can only minimize the signs of inflammation like is shown in a study from Lee and colleagues (2005).
When a tissue is injured, the cardinal signs Rubor (redness), Calor (heat), Edema (swelling), Dolor (pain) and Funca Laesa (functional loss) will occur to some degree, and the body responds with the inflammatory response.
The healing phases associated are:
- the inflammatory phase (acute care),
- the proliferation phase (sub-acute care) and
- the maturation phase (post-acute care).
In each of these phases, the way local cryotherapy should be applied is different and even finds a transition point, the point where no longer cryotherapy but local heating should be utilized. The complete process needs to be driven by clinical decision making; a proper physical examination, a patient interview and notice of the response to prior treatment.
The goals of cryotherapy during your rehabilitation in the different phases are:
- Facilitating rehab exercises
- Pain management
- Limit analgesic use
- Limit arthrogenic muscle inhibition
While to increase effectiveness, the appropriate cryotherapy duration should be determined by measuring the skinfold thickness at common cryotherapy treatment sites (Jutte et al. 2012). This dependency on skinfold thickness is also illustrated in figure 1; a larger adipose tissue implies longer treatment durations to become the same tissue temperature drop.
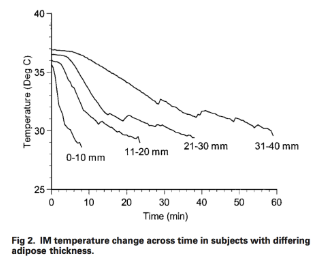 (Figure 1; derived from Otte et al. 2002).
(Figure 1; derived from Otte et al. 2002).
In time the cryotherapy strategy (ICE), transferred into RICE (rest and cooling), into PRICE (Protection, Rest and cooling). Bleakley and colleagues (2012) after that, suggested POLICE, a new acronym, which represents protection, optimal loading, ice compression, and elevation. In this approach, optimal loading is integrated, as new insights consistently provide evidence that mechanical loading upregulates key proteins associated with soft tissue healing.
Besides new scientific insights, new technologies are developed and available on the market. These technologies make it possible to break with “the 20 minutes habit” thereby being able to cool down intra-articular temperatures. While other technologies, like cryogenically cooled air, can decrease superficial tissue temperature more rapidly by the use of much colder temperatures (up to –140°C or -220°F).
These new technologies will help to make the use of cryotherapy more effective. It should be remembered though (according to Bleakley et al., 2004) that:
- An optimal tissue temperature reduction of 10°C to 15°C is necessary to maximize the therapeutic effect.
- The skin temperatures should drop to below 13,6°C to achieve local analgesia and
- A tissue temperature between 10°C and 15°C may be required to maximally lower metabolism.
Based on all this, what’s new in the use of local cryotherapy?
- ICE-> RICE->PRICE-> POLICE, position local cryotherapy in an integral approach that also focusses on optimal loading.
- In the acute care phase, the focus should be on applying local cryotherapy which shifts to optimal loading in the proliferation phase and maturation phase where local cryotherapy only assists.
- Clinical decision making should determine the transition point from applying local cryotherapy to local heating.
- New technology, using very low temperatures, make local cryotherapy more efficient.
- Local cryotherapy should be customized taking body composition, gender, and fitness into account.
In summary, the duration, intensity, and frequency of local cryotherapy should be determined by the repair phase, the injured tissue, depth of injury, personal characteristics and cooling modality. The new technologies for local cryotherapy can be applied in other domains than sports or rehabilitation as well as for vitally or beauty needs. In these domains the workings mechanisms are different, but the general principles remain.
References
- Bleakley, C. M., Glasgow, P. & MacAuley, D. C. PRICE needs updating, should we call the POLICE? Br J Sports Med 46, 220–221 (2012).
- Bleakley, C., McDonough, S. & MacAuley, D. The Use of Ice in the Treatment of Acute Soft-Tissue Injury A Systematic Review of Randomized Controlled Trials. Am J Sports Med 32, 251–261 (2004).
- Jutte, L. S., Hawkins, J., Miller, K. C., Long, B. C. & Knight, K. L. Skinfold Thickness at 8 Common Cryotherapy Sites in Various Athletic Populations. J Athl Train 47, 170–177 (2012).
- Lee, H. et al. Effects of cryotherapy after contusion using real-time intravital microscopy. Med Sci Sports Exerc 37, 1093–1098 (2005).
- Otte, J. W., Merrick, M. A., Ingersoll, C. D. & Cordova, M. L. Subcutaneous adipose tissue thickness alters cooling time during cryotherapy. Arch Phys Med Rehabil 83, 1501–1505 (2002).





